Another One Bites the Dust
by Kristin Rowan, Editor
Essentia Drops Medicare Advantage
Essentia Health is an integrated health system with locations in Minnesota, North Dakota and Wisconsin. The health system offers 285 different services across more than 1,700 locations. They employ more than 2,700 doctors. Essentia also includes 14 hospitals, emergency care, same-day care for mental health crises, and multiple specialties.
This is all to say that Essentia Health is not a small player. They contract with the largest payers in the industry.
Re-Evaluation
“This was not a decision we made lightly. The frequent denials and associated delays negatively impact our ability to provide the timely and appropriate care our patients deserve. This is the right thing to do for the people we are honored to serve.”
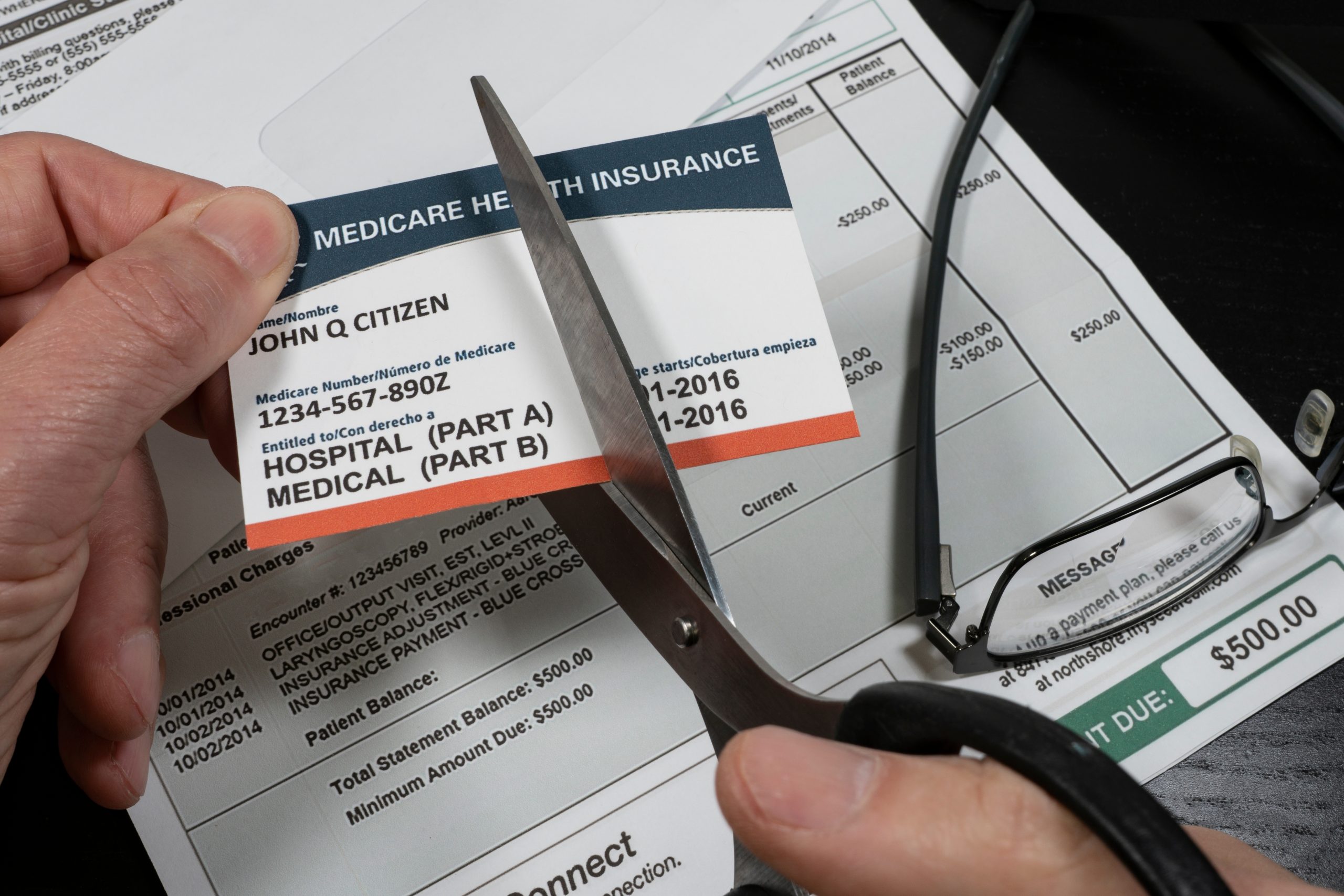
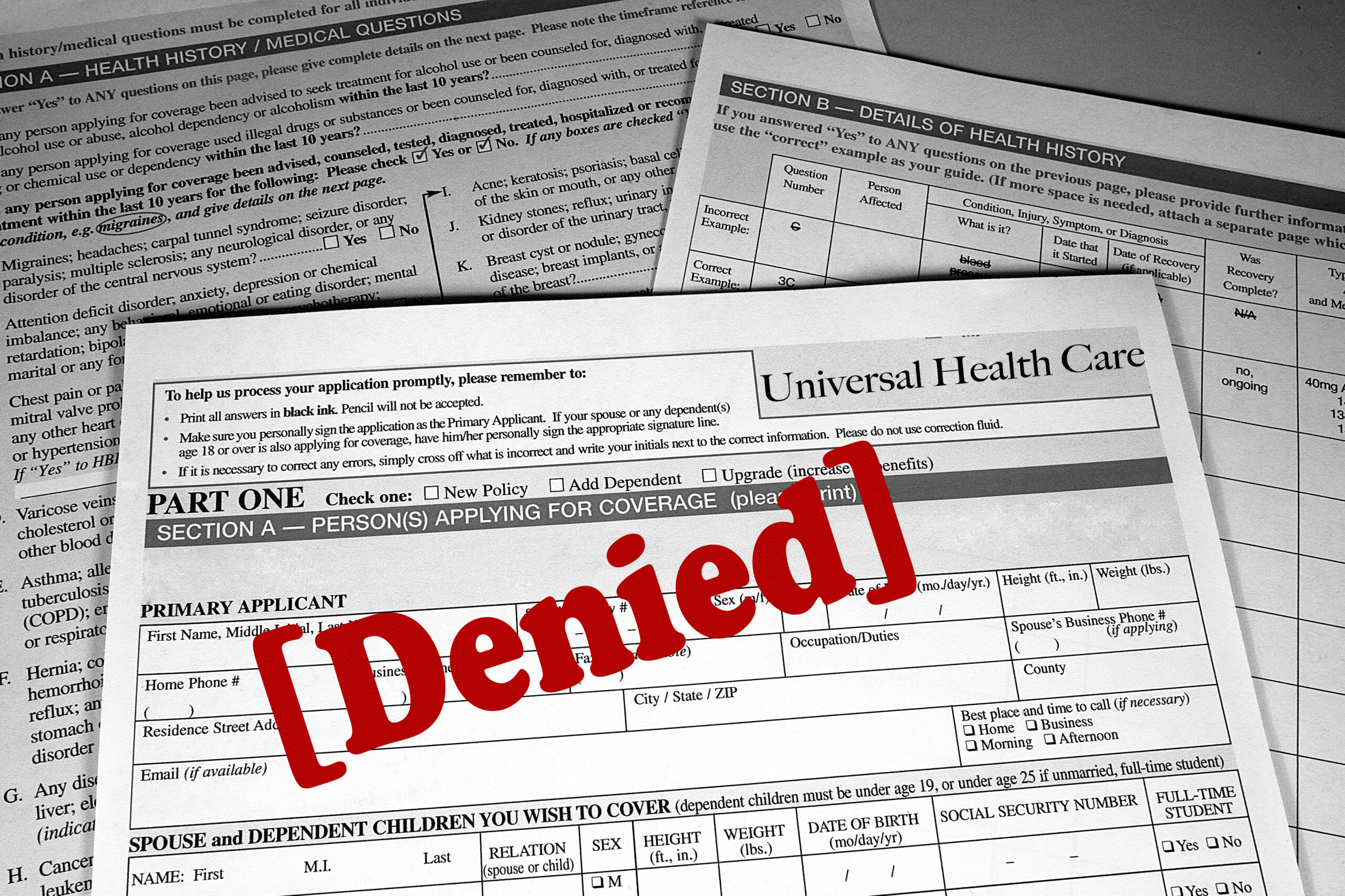
Essentia informed patients that they will no longer be an in-network provider for MA plans through UnitedHealthcare (UHC) or Humana beginning January 1, 2025. The health system claims that UHC and Humana delay and deny approval of care at more than twice the rate of other Medicare Advantage plans. They are encouraging its patients to choose a different plan during open enrollment that is in-network with Essentia.
UHC Responds
UnitedHealthcare responded to the press release that Essentia issued. According to their statement, the two parties extended their contract just this past July. Negotiations included a number of items on which they agreed to collaborate, but Medicare Advantage was not specified among them.
“Essentia Health didn’t raise concerns regarding its participation in our Medicare Advantage network until last week. We have since met with Essentia on Sept. 9 and are committed to working with the health system to explore solutions with the goal of renewing our relationship. We hope Essentia shares our commitment toward reaching an agreement.”

Following Suit
Essentia’s departure from Medicare Advantage is just one in a recent mass exodus.
Sanford Health of South Dakota ended its Humana MA participation due to “ongoing challenges and concerns that negatively effect patients including ongoing denials of coverage and delays in accessing care.”
HealthPartners out of Minnesota announced over the summer that “UnitedHealthcare delays and denies approval of payment for MA claims at an exceptionally high rate…up to 10 times higher than other insurers…. After over a year of being unable to persuade UnitedHealthcare to change their practices, we’ve determined that we can no longer participate in the UnitedHealthcare Medicare Advantage network.”
Mercy, the official medical provider of the St. Louis Cardinals, announced its year-end departure from the Anthem Blue Cross Blue Shield network. This includes all Medicare Advantage, ACA marketplace, and managed Medicaid plans. They cited administrative tasks that create a barrier to timely, appropriate patient care. Mercy also complained that Anthem has raised its rates for patients and employers, increased its profits, and still has not raised reimbursement rates to providers. Like Essentia, Mercy is encouraging its patients to consider whether the health care plan they choose during open enrollment will list Mercy as one of its in-network providers.
Final Thoughts
CMS reimbursement rates, Medicare Advantage denials, payment delays, and other interruptions are impeding patient care. As Tim mentions in his editorial this week, we are in an election year and we urge you to research how each party might impact our industry.
If more providers and payors continue to drop Medicare Advantage from their offerings, will we see more patients returning to traditional Medicare plans with an affordable Medicare Supplement or MediGap coverage? One can only hope!
# # #


Kristin Rowan has been working at Healthcare at Home: The Rowan Report since 2008. She has a master’s degree in business administration and marketing and runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in event planning, sales, and marketing strategy. She has recently taken on the role of Editor of The Rowan Report and will add her voice to current Home Care topics as well as marketing tips for home care agencies. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
©2024 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in Healthcare at Home: The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com


 The financial and health implications of uninformed disenrollment from PACE to conventional MA plans are significant. The needs of PACE beneficiaries, most of whom have multiple complex medical conditions, cognitive or functional impairments – or all three – are not comprehensively addressed by MA plans. The loss of PACE services is harmful and, in some cases, can be life-threatening.
The financial and health implications of uninformed disenrollment from PACE to conventional MA plans are significant. The needs of PACE beneficiaries, most of whom have multiple complex medical conditions, cognitive or functional impairments – or all three – are not comprehensively addressed by MA plans. The loss of PACE services is harmful and, in some cases, can be life-threatening. We share CMS’ stated desire that people have access to accurate and complete information when they make health care choices. We have numerous examples of vulnerable seniors being induced to enroll in MA plans without being fully-informed of what they are giving up when they enroll.
We share CMS’ stated desire that people have access to accurate and complete information when they make health care choices. We have numerous examples of vulnerable seniors being induced to enroll in MA plans without being fully-informed of what they are giving up when they enroll.